Gut Health and Mental Health
The connection between gut health (microbiome) and mental (brain) health.
Dr. Mason Bresett ND naturopathic doctor located in Sarnia, Ontario discusses how gut health can impact mental health.
More than 2000 years ago, Hippocrates stated, “all disease begins in the gut”
Disorders of gut brain interactions are on the rise. There is no question that our mental health is impacted by our gut health, diet, lifestyle and digestion. If your health care provider suggests differently, I would consider a second opinion. The objective of this article is to discuss how this happens, why this happens and what to do about it.
Think about this before you read the article. Your microbial genome (genetic pool) is bigger than yours. You have roughly the same amount of bacterial “non-human” cells in your body as human cells. This ratio is about 1:1.
It is widely accepted that a gut microbiome exists, it is less known that the eye, skin, vagina, mouth and possibly even a brain microbiome exist. Our gut microbiome is the main “biome” especially when relating to mental health. The secondary biomes are highly dependent on the health of the gut microbiome.
Before we move on to how this all works let’s go over some key terms and descriptions:
Gut Health: the importance of a healthy diet + microbiome and being able to have a strong immune system, plus properly digest and absorb nutrients.
Microbiome: the collection of all microbes, such as bacteria, fungi, viruses, and their genes, that naturally live on our bodies and inside us
Mental Health: our emotional, psychological, and social well-being. The tendency for some to experience overwhelm, anxiety, depression, panic, obsessive compulsive behaviours and other psychiatric disorders.
Microbiota-gut-brain-axis (MGBA): the connection between the microbiome, gut and brain.
Prebiotics: molecules that provide fuel and nutrition for beneficial bacteria in the microbiome, they need to be broken down by bacteria as the human digestive system can’t do so.
Probiotics: a substance that promotes balance in the microbiome which can be a food or a supplement.
Post-biotic: by-products of the breakdown products of bacterial fermentation and digestion such as short chain fatty acids like butyrate and vitamins.
Microbiome Gut Brain Connection
An example of how infectious disease and microbiome-immune alteration can impact mental health can be seen with group A beta-hemolytic streptococcal infections. Some patients who get strep infections can go on to develop obsessive compulsive disorder (OCD). This is commonly seen in individuals diagnosed with PANDAS and PANS in our clinic (20).
Research suggests that inflammation at the gut level can impact our brain and psychological stress can impact the gut. Functional MRI’s have shown that those who suffer from digestive disorders show different brain patterns in regions associated with mental health concerns like depression (1). This research also highlights that syndromes like IBS have a correlation with Dementia, Alzhiemer’s and Parkinson’s Disease.
Stress induced leaky gut and leaky brain
Chronic stress can impact gut health due to hypothalamus-pituitary and adrenal (HPA) axis dysregulation. This is the chain of events starting from the brain to organs associated with stress response. With some HPA axis concerns, cortisol (our main stress hormone) can increase intestinal permeability (leaky gut), this is when the barrier between your gut becomes compromised (think large pores that shouldn’t be there). If unchecked, this creates pro-inflammatory responses that can make it all the way to the brain, causing neuro-inflammation, (brain inflammation). How do you think a brain feels if it is inflamed? With alarming rates of brain fog patients coming to our clinic, I think there may be a connection here.
Probiotic studies have shown reductions in stress hormones and stress highlighting the impact our gut can have on stress..(16-18). Stress is not the only thing that drives this cascade, but a good example due to its prominent presence in society. This highlights the connective nature of the microbiota-gut-brain axis (2,19).
Unresolved trauma, trapped survival stress and emotions are barriers to a healthy microbiome-gut-brain axis. 50% of IBS patients have trauma according to some research (1). Most people know that our stress can trigger fight or flight mode. Yet the 3rd “freeze phase” is often under-appreciated. The freeze response puts a “shutdown” on the nervous system (if you can’t fight or flee you will keep yourself small). This traps the fight or flight survival energy in your system. This is like having your nervous system brake and gas on at the same time. This suppression causes an enormous amount of energy to be used up including our most anti-inflammatory hormone, cortisol. This can impact our HPA axis and create digestive and mental health symptoms as we can’t rest, digest and heal, especially our gut lining. The above is a summary from Irene Lyon’s resources on the polyvagal theory and functional freeze. Our inner nature is to become self regulated. Nervous system dysregulation is a leading cause of digestive issues which can have impacts on our mood and mental health.
In our clinic we utilize adaptogen herbs alongside customized treatment plans to help reduce impacts of stress on the body and the gut brain axis. These are a class of herbal medicines that help increase resiliency to stress to protect the MGBA from cortisol dysregulation.
Stress also lowers stomach acid levels. Stomach acids are needed to break down food and microbes that enter the gut via the mouth. Stomach acids also are needed to trigger certain enzymes needed for digestion. This is a smart design by the body, because our bodies won’t prioritize digestion if we are sending our blood and survival energy to our limbs and muscles.
The vagus nerve is an important nerve that runs from your brain stem to many vital organs including our gut. 80% of this nerve is sensory meaning the majority of the information is coming up your microbiome and gut to your brain. Although simplified, this suggests our interoception and learning to sense the wisdom and impulses in our body is vital. Stress comes in many forms but often from overexertion and lack of consistent nervous system relaxation.
Boundaries and Leaky Gut
The gut wall is a single-cell layer connected by proteins. These proteins are impacted by diet, inflammation, toxins and stress. If impacted too much, a process called “leaky gut” or intestinal permeability occurs. Leaky gut sets the stage for chronic inflammation to travel from the gut systemically to the body and brain, which may impact mood. This boundary is important because it is a vital interface that the body uses to distinguish self (my body) from non-self (invader).
Naturopathic doctors discovered this process in the 1900’s only to be discredited by medical science “experts” calling the shots on the narrative around what is true. Later, a Harvard gastroenterology researcher, named Dr. Fasana MD, put leaky gut or intestinal permeability on the map as a legitimate medical concern. When the gut suffers damage, a protein called zonulin is released which causes damage to the lining of the digestive system (see more on this in the testing option section below). The standard Canadian diet sets someone up to have a greater chance of suffering from a leaky gut.
Gut and Mood
The human gut has 6 main phyla or groups of bacteria that account for 90% of total flora.
Lactobacillus and Bifidobacterium are two common species in babies, breast fed babies and vaginal born babies. These two strains are commonly researched in depression, as low levels may be associated with major depression disorder (2). In a study tracking depressed patients, 70% had digestive symptoms and there was a correlation between the severity of the symptoms and their depression levels (3).
“A higher frequency of digestive symptoms was associated with an increased risk of suicide ideation, suicide attempts, anxious mood, depressed mood, insomnia, feeling a failure, poor concentration, body pain, hopelessness, anger, and irritability” (4). This quote from the study highlights something I have heard about or witnessed in our local clinic and community.
One study showed 70-90% of Irritable Bowel Syndrome patients also had mental health symptoms (5). Another study showed 84% of participants had anxiety and 24% had depression who were also diagnosed with a gut disorder (6). A psychiatrist in Ireland, Dr. Dinan noticed his depressed patients also had gut health issues. He later coined the term “Psychobiotics” which are probiotics, when ingested in adequate amounts, produces a health benefit in patients suffering with mental health symptoms plus stress and immune related disorders (8). Prebiotics are also important as they ensure growth of the bacteria that support mental health effects.
When medicine was more heroic and invasive, surgeries were performed to cut the connection between the vagus nerve in patients suffering from ulcers. What’s interesting is that none of these patients went on to develop Parkinson’s Disease (7). This highlights the possible connection between what researchers have found in regards to poor gut health being a potential trigger for conditions like Parkinson’s or neurological disorders.
Neurotransmitters
Neurotransmitters are chemical messengers that shape our mental health architecture. The most common include: dopamine, serotonin, norepinephrine, acetylcholine and GABA. These are imperative to mood, focus, memory and more. It is estimated that 90-95% of serotonin and 50% of dopamine are in the gut and outside of the brain. Research is still being done to determine how gut levels of neurotransmitters impact brain levels.
This is a short generalization of what these neurotransmitters do and is not comprehensive.
Serotonin: mood, emotions and digestion
Dopamine: mood, learning, movement and used to make norepinephrine
Norepinephrine: arousal, attention and stress
Acetylcholine: memory, motivation and attention
GABA: mood and impacts on calming the system
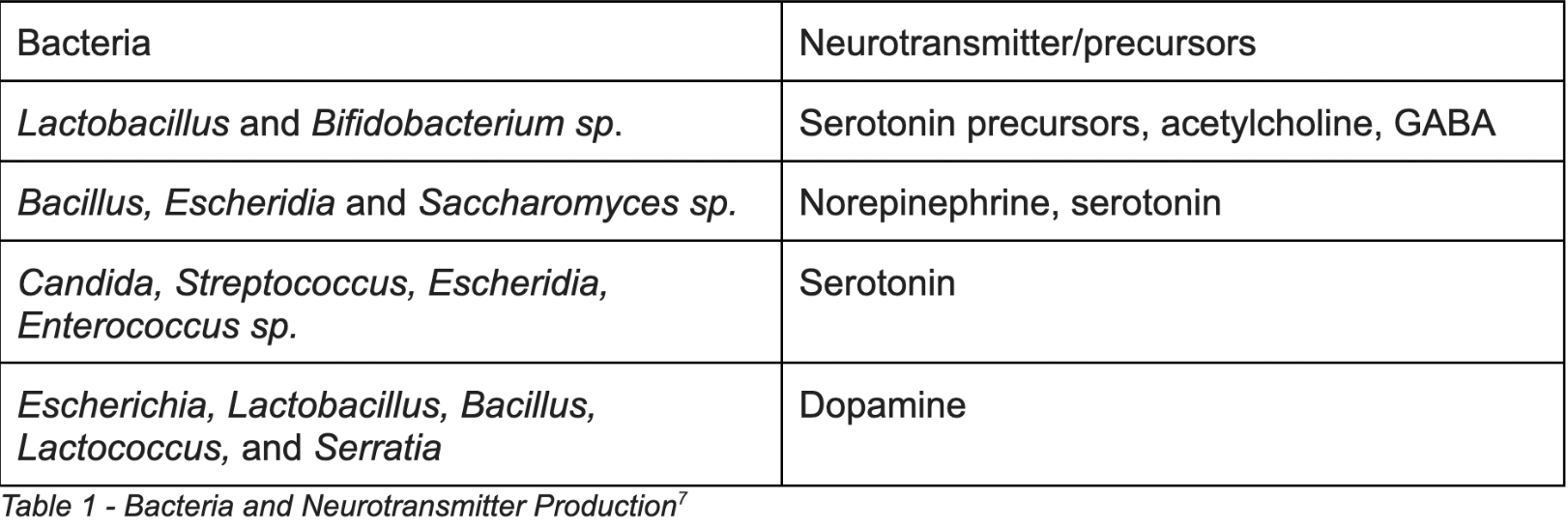
Preliminary research suggests that certain bacteria can synthesize neurotransmitters and building blocks for them seen in table 1 below (7).
The combination of Lactobacillus and Bifidobacterium species have been used in multiple studies showing decreased anxiety and depression. The researchers infer these bacteria impact serotonin and GABA hence impacting mood regulation (8-15). Improved scores on standardized depression rating scales were improved in those receiving probiotics. These studies also showed an increase in brain-derived neurotrophic factor (BDNF). Brain-derived neurotrophic factor (BDNF), a neurotransmitter modulator which is assumed to help brain health and neuroplasticity.
An important connection to make here is that all of these neurotransmitters require amino acids as building blocks. Amino acids are what combine to make protein. Protein deficiency can lead to altered mood and neurotransmitter balance. Another factor that can inhibit this other than low intake include: low stomach acid, a very common condition. Without adequate stomach acid, protein and mineral absorption is limited. Stomach acid blocking medications may inhibit the proper digestive function needed for amino acids.
Infections and Mental Health Risk
Gastrointestinal and respiratory infections increase the future risk of anxiety disorders (21). This may be due to microbiome-gut-brain alterations or mainly triggered by medication given like antibiotics. As a naturopathic doctor this makes me want to continue supporting my patients with health creation strategies to 1) improve their baseline immune function (terrain) to prevent infections 2) treat acute infections as a way to inform the immune system not weaken it. Ask about our fever and acute infection course for more info on this topic. In essence, the body’s immune response during acute infections is a natural way to move through an infection or disturbance in health with some sort of discharge (mucus, fever, pain). Sometimes medications are needed, but the more we just use that approach for cases that could resolve naturally with naturopathic acute management, the less immune development we get and this can lead to more biofilms and resistant bugs -not to mention the planetary impact of these agents.
Bloating, Urgency and Constipation
Gut symptoms like bloating, urgency and constipation are a sign that something is up with the gut-microbiome-brain axis. Subtle infections and alterations in the microbiome can also cause absorption issues and impact mental health. For example, a large percentage of IBS sufferers may actually have small intestinal dysbiosis or Small Intestinal Bacterial Overgrowth (SIBO) (22).
This is when your small intestine has more bacteria than what’s deemed healthy. As mentioned above, bacterial overgrowth is one of the key inducers of leaky gut. This condition can cause bloating, loose stools/diarrhea, constipation, malabsorption and mental health symptoms due to gut alteration and nutrient deficiency.
Children
Children’s mental health can look different from adult mental health. Conditions like autism, ADHD, food restriction/picky eating, insomnia, sensory disorders and behavioural issues often have links to the microbiome-gut-brain-axis.
The Other Ones
Although a lot of this article has been targeted towards bacteria, other microbes like fungal organisms and parasites can be an issue. For instance, a fungal yeast also known as Candida albicans is a naturally occurring fungus in our gut - yes that's right we have our own mycobiome as well, a collection of yeasts that can support or harm us. When this gets out of balance as seen in certain gut conditions like Crohn’s Disease and Ulcerative Colitis, negative outcomes emerge (23,24)
Another systemic issue that impacts the microbiome-gut-brain axis are mycotoxins. Mycotoxins are biotoxins from mold or water damaged buildings or environments. This is especially common in south western Ontario due to the humidity levels and Great Lakes weather patterns. These toxins from mold can mess with our nervous system and detoxification systems like our autonomic nervous system, colon, lymph, liver-bile system and kidneys (25-27).
Although parasites are trending as the “cause of everything wrong with me” on the internet right now - they can cause issues but usually not the first place to start looking. For example, parasites usually accompany a gut with a travel history or heavy metal and toxin burden.
Risk Factors
There are many factors that can impact the microbiome-gut-brain-axis such as:
Medication and antibiotic use
Diet
Stress
Gluten and Gliadin (wheat proteins) for some people
Birth delivery type
Birth location
Poor dental health
Recurrent infections including subtle dental infections
Breastfeeding history
Environmental toxins (especially glyphosate and mycotoxins)
Adverse childhood experiences (ACES) and nervous system dysregulation
Chlorinated and forever chemical laced water
Health Creation Map for A Healthy Microbiome, Gut and Brain
Nutrition/Digestion
An anti-inflammatory whole foods diet can be supportive of a healthy microbiome-gut-brain axis. Some ideas to consider include:
Nutrition plans: mediterranean diet, paleo diet, plant-focussed diet or simply eliminating processed foods.
Prebiotic foods include: mushrooms, jicama, dandelion greens, asparagus, artichokes, cooled starches, kiwi, endives, pomegranates, beans and more.
Probiotic foods: yogurt, sauerkraut, lacto-fermented pickles and veggies, low sugar kombucha, tempeh and kimchi.
Ample protein for neurotransmitters. 1 g per kg is a good starting place for most. Some folks need more than this (athletes, certain health conditions, etc)
Diverse and ample fiber intake will increase short chain fatty acids (SCFA) which can help support the digestive system and microbiome gut brain connection. Eat the rainbow, enjoy whole grains and avoid eating the same thing day after day.
The Bitter Truth
There are more flavours in the human diet than sweet, salty and umami. Bitter and sour are two of the lesser utilized flavours in standard Canadian cooking. Bitter foods are incredible tonics for the digestive system. Bitters (for short), help increase natural stomach acid production, help modulate blood sugar and increase enzyme production. Having a bitter salad, apple cider vinegar or herbal bitters before meals was and is a time tested method to support digestion and absorption.
Probiotics
If buying probiotics on the market, the ones in the fridge aren’t more supreme but if one says keep it in the fridge, do so. Read directions as the guaranteed bacterial count is based on their temperature recommendations. Try to focus on probiotics that have been studied for mental health concerns.
Look for third-party tested probiotics to ensure quality and purity. They should also be manufactured at cGMP-compliant facilities, meaning the facility must meet requirements set forth by Health Canada.
At our clinic we use a combination of probiotics, soil based probiotics, prebiotics, polyphenols and antimicrobials to support individuals. The potency (millions-billions), also known as colony forming units (CFU), is chosen based on patient needs. This is often adjusted as things change and eventually we shift patients to probiotic foods when their job has been done.
Sometimes probiotics are not indicated and can actually make things worse at certain phases of one’s health care plan.
Stress
Create a measurable and accountable stress reduction plan. If you feel like you are in shutdown or functional freeze or any other state that doesn’t feel optimal for you - ask your naturopathic doctor for ideas and referrals on who/what can help get you unstuck. Prioritizing sleep and circadian rhythm balance helps our gut-brain axis. Remember to listen to your gut :)
Environment
Do what you can to lessen the impact your environment has on your gut. If you can, get a water filter, seek out chemical free food and reduce household toxic exposures whenever possible. Herbicide, and pesticide exposure, especially glyphosate (round-up), can have a slow but impactful assault on the gut. Detoxification and buffering strategies are recommended for overall health.
Infections
Strengthen your immune system with preventive immune support. If suffering from an acute infection we offer acute naturopathic medical visits to treat infections with naturopathic principles. Get a check-up to assess for chronic infections that can impact mental health or neurological health long term. Note: we refer when emergent or differing expertise is necessary.
Exercise
The impact of exercise is vital for both digestive and mental health. Try to find a balance as under exercising and over exercising can be detrimental to the microbiome-gut-brain-axis.
Medications
If using antibiotics or other medications that impact your microbiome consider talking to your health care provider about replacing healthy bacteria at the recommended timing with indicated probiotic strains.
Note individuals who have reactions to penicillin or other mold based antibiotics may have mycotoxin illness.
Testing Options for Microbiome-Gut-Brain and Mental Health
SIBO breath testing - a digestive breath test for those with bloating and IBS like pattern
Micronutrient testing - vitamin and mineral testing to assess malabsorption
Comprehensive Diagnostic Stool Analysis with zonulin - a complete stool test to map the microbiome which assess digestive function, short chain fatty acid production and leaky gut markers
Organic Acids Testing - a urine test which assess neurotransmitter and digestive markers of yeast and bacteria imbalance
Food Intolerance / Sensitivity Testing - assessments to determine if foods in current diet are negatively impacting the body
Burp and Acid Test - In house procedures recommended to assess for stomach acid levels
Heart Rate Variability (HRV) - HRV assessments can be supportive in determining stress load
Not all of these tests are recommended. But sometimes one or multiple are chosen to gain objective data to folks suffering from mental health concerns.
Summary
The microbiome gut brain axis can impact mental health symptoms in so many different ways. By learning the basics, I hope this article provides some education into a trending area. Education is key when making health care choices for you and your loved ones. If you are suffering from mental health concerns, consider a naturopathic medical initial visit. Naturopathic doctors treat the whole person and not just the symptom.
The disclaimer… The amazing thing about humans is that we all have incomparably unique health profiles and needs. The health-related information contained in this article is intended to be general in nature and should not be used prescriptively or as a substitute for a visit with a naturopathic doctor/health care provider. This info is intended to offer general information to individuals. If you have questions about how these strategies could be used in adjunct to your current health regime, book an appointment with us or consult a licensed naturopathic doctor for individualized care.
References